Difference Between Lactic Acid & Lactate
By Andrea Cespedes
You'll hear "lactic acid" and "lactate" used interchangeably by trainers, coaches and other sports experts. Colloquially, people assume you mean the same thing when you use either term, but they are technically different. Lactate is produced by your body in response to aerobic exercise and serves as a fuel for the muscles, delays fatigue and prevents injury. Lactic acid contains one additional proton and is not produced by the body at all during exercise.
One Proton
The technical difference between lactate and lactic acid is chemical. Lactate is lactic acid, missing one proton. To be an acid, a substance must be able to donate a hydrogen ion; when lactic acid donates its proton, it becomes its conjugate base, or lactate. When you're talking about body's lactate production and lactate or lactic acid threshold, the difference is largely a matter of semantics. But, the body produces and uses lactate -- not lactic acid.
What Is Lactate?
During hard exercise, from running a race to surfing the waves, your breathing rate increases to deliver more oxygen to the working muscles. Some exercises are so intense -- such as lifting a heavy dumbbell or swimming away from a shark -- that your body cannot use oxygen fast enough as a source to create fuel. For these quick, intense bursts of activity, your body needs to move into anaerobic mode -- during which the stored energy in your body is broken down into a compound called pyruvate.
When you don’t have enough oxygen to perform activity, your body turns pyruvate into lactate to fuel the muscles. Fit folk can utilize this form of energy production for one to three minutes.
High Levels of Lactate
As the muscles work at intense levels, they become more acidic, which interferes with firing. Lactate isn't the cause of this acidity; it's actually an antidote to this muscle failing. As your muscles lose power and energy, lactate swoops in to help counteract the depolarization of the cells. This is the familiar burn in the muscles you feel when you just can’t do another rep. Lactate production is a protective mechanism that prevents the body from hurting itself. When lactate production can't continue to the levels needed to prevent the complete failure of the muscles, you reach your threshold.
High levels of lactate -- or, as it is sometimes called, lactic acid -- were once blamed for delayed-onset muscle soreness. Lactic acid or lactate are not responsible for the soreness. Rather, researchers believe it is due to micro tears in the muscles that occur during strenuous exercise.
A Measure of Athletic Success
Lactate is essential to the exercising process. It helps bolster the mitochondria, energy powerhouses inside each of your muscle cells. Increase the number of mitochondria in your cells, and you'll improve your stamina and strength. High-intensity interval training in which you do short bouts of very strenuous exercise at or near your lactate threshold followed by recovery is especially effective in developing your lactate threshold. The better able you are to process lactate, the greater your ability to push high levels of performance.
About 75 percent of the lactate you produce during exercise is used as this moderating energy source; the other 25 percent leaks into the blood, which is how scientists test lactate levels during exercise. At one time, it was thought that high-level athletes produced less lactate; it's more likely that these athletes are better able to utilize the lactate they produce and leak less into the bloodstream, so their tests show lower amounts.
The Liver & Detoxification (Part 1)
By Graeme Bradshaw
Did you ever want to know about how to look after your liver?
This is part of a detailed series of articles explaining liver metabolism related to detoxification. You will learn how and what to do to maintain optimal liver health.
Where is the liver?
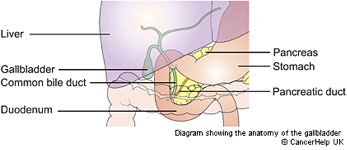
The Liver’s location is on the right side, at base of the ribs, shown in lilac color. The Gall Bladder sits under the liver.
Expanded view of the gall bladder ducts - the gall bladder is under the liver
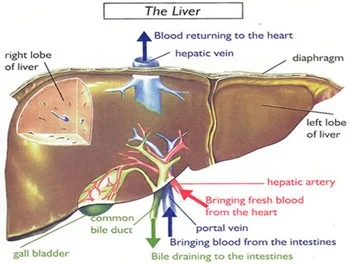
The next diagram gives a better idea of the actual appearance of the liver, as well as how the blood flows into it from the intestines. It is the first place blood that having picked nutrients, like fats, amino acids, phyto-chemicals, vitamins and minerals and any wastes from the intestines and bowels. One of the liver's primary functions is filtering the blood. Almost 4 liters of blood pass through the liver every minute for detoxification. The blood then passes out to the heart.
Bile from the liver is both a waste product, and it helps digesting and absorbing the fats and oils form food. Bile is especially released by fatty meals. Bile is necessary for bowel peristalsis, that is constipation may be caused by lack of bile.
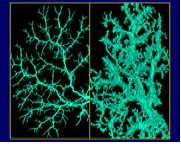
Green colors above indicate the “biliary tree”, which are the bile ducts draining the liver into the gall bladder. These may be blocked with fatty cholesterol-laden plaque, bilirubin and bile salts, as depicted on the picture on the right side. The gall bladder may become congested with this plaque if it is not released as well and is prone to crystallize into gall stones by mid-life if the diet is incorrect. Read on for how to prevent this.
What are the functions of the liver?
- It is responsible for the production of bile that is stored in the gallbladder and released when required for the digestion of fats
- The liver stores glucose in the form of glycogen that is converted back to glucose again when needed for energy
- It also plays an important role in the metabolism of protein and fats.
- It stores the vitamins A, D, K, B12 and folate and synthesizes blood clotting factors.
- Another important role is as a detoxifier, breaking down or transforming substances like ammonia, metabolic waste, drugs, alcohol and chemicals, so that they can be excreted. These may also be referred to as "xenobiotic" chemicals.
Filtering the Blood
The liver plays a key role in most metabolic processes, especially detoxification. The liver is a filter designed to remove toxic matter such as dead cells, microorganisms, chemicals, drugs and particulate debris from the bloodstream. The liver filter is called the sinusoidal system, and contains specialized cells known as Kupffer cells that are part of the white blood cell immune function. They make up 10% of liver weight, and function to ingest and break down toxic matter.
Filtration of toxins is absolutely critical as the blood from the intestines contains high levels of bacterial waste, (endotoxins from the bowels), antigen-antibody complexes, and various toxic pollutants. When working properly, the liver clears 99% of the bacterial toxins during the first pass. However, when the liver is damaged, such as in alcoholics, the passage of toxins increases by over a factor of 10. This is similar if your intestines are too permeable, a condition known as “leaky gut”. Allergies (especially to gluten) and parasites may cause this.
The liver neutralizes a wide range of toxic chemicals, both those produced internally and those coming from the environment. The normal metabolic processes produce a wide range of chemicals and hormones for which the liver has evolved efficient neutralizing mechanisms. However, the level and type of internally produced toxins increases greatly when metabolic processes go awry, typically as a result of nutritional deficiencies, pesticide laden foods, low fiber diets and high red meat or alcohol intake.
Many of the toxic chemicals the liver must detoxify come from the environment: the content of the bowels and the food, water, and air. The polycyclic hydrocarbons (DDT, dioxin, 2,4,5-T, 2,3-D, PCB, and PCP), which are components of various herbicides and pesticides, are on example of chemicals that are now found in virtually all fatty tissues of the body, including the brain. Even those eating unprocessed organic foods need an effective detoxification system because all foods contain naturally occurring toxic constituents, and bacterial or fungal activity in the bowel may produce more.
So far we’ve learned that liver plays several roles in detoxification: it filters the blood to remove large toxins, synthesizes and secretes bile full of cholesterol and other fat-soluble toxins, and now we move on to how it enzymatically disassembles unwanted chemicals. This enzymatic process usually occurs in two steps referred to as phase I and phase II. Phase I either directly neutralizes a toxin, or modifies the toxic chemical to form activated intermediates that are then neutralized by one of more of the several phase II enzyme systems.
Proper functioning of the liver's detoxification systems is especially important for the prevention of cancer, since phase II detoxification deactivates carcinogens. Around 70% of all cancers are thought to be due to the effects of environmental carcinogens, such as those in pesticides, trans and burned fats in food, plastics and other sources of environmental estrogens, as well as air pollutants, cigarette smoke, etcetera. Our own hormones that are poorly detoxified may be cancer inducing, notably some forms of estrogens, and we are especially at risk if there is insufficient liver detoxification and bowel elimination. When combined with deficiencies of the nutrients the body needs for proper functioning of the detoxification and immune systems this issue gets worse. The level of exposure to environmental carcinogens varies widely, as does the efficiency of the detoxification enzymes, particularly phase II. High levels of exposure to carcinogens coupled with slow phase II detoxification enzymes significantly increases susceptibility to cancer.
Bile Excretion
The liver's second detoxification process involves the synthesis and secretion of bile. Each day the liver manufactures approximately 2 liters of bile, which serves as a carrier in which many toxic substances are dumped into the intestines. In the intestines, the bile and its toxic load are absorbed by fiber (if there is any in the diet) and then excreted. However, a diet low in fiber results in inadequate binding and reabsorption of the toxins back from the intestines into the liver. This low fiber diet (especially soluble fiber like oats and flax seed lignans) is a major cause of gall stones. This problem is magnified when bacteria in the intestine modify these toxins to more damaging forms.
The Gall Bladder : What does it do?
The gallbladder's main purpose is to concentrate and store your bile. Bile is a fluid made in the liver that helps you to digest fats in your small intestine. It is made from cholesterol, water, bilirubin and bile salts.
Bilirubin is what gives bile its greenish colour – the color turns darker brown the longer it is in the intestines. Bilirubin comes from the breakdown of used red blood cells.
When you eat fatty foods, the fats are broken down (digested) in your stomach and intestines. To get the bile to the food in your gut, your body either:
- Releases it from the liver and down the bile ducts, straight into your small intestine
- Stores it first in your gallbladder, which releases bile into your common bile duct as you need it
- Fats and oils in the diet stimulate the release of bile following a meal
- Fiber, especially soluble fibre such as from oats causes more bile to be released from the bowel, reducing gall stone formation. A low fiber diet increases gall stone risks, especially if no breakfast is eaten.
Factors causing most gallstone formation:
- A low fiber diet. Low fiber from too few vegetables, fruits, and whole-grain foods and whole grains such as oats or flax seeds. Do you eat 5 serves of fruit and vegetables a day or have a high fiber cereal breakfast? If not add oats and flax seeds which have high lignan content that is a soluble fiber.
- Too much red meat, cheese, and other dairy, bacon, sausages and gravies which are all high in saturated fat, that increase triglycerides (TG’s) and cholesterol, affecting the liver and gall (makes more concentrated bile).
- Omega 3 oil deficiency makes the TG’s and cholesterol go higher as well. Omega-3 oil, found in fish or flax seed oil, blocks cholesterol formation in bile.
- Sugar (and lack of exercise) increases triglyceride (TG’s) levels in the blood – high TG’s create less soluble bile. High sugar intake increases insulin levels that increase cholesterol saturation in bile (a bad effect).
- Irregular meals, skipping breakfast (“coffee breakfast”) and crash dieting contribute.
- Estrogens (the pill and oral contraceptives, and pregnancy increase frequency of gall stones – hence women more common sufferers). Women with a family history of gallstones are best to avoid oral contraceptive pills.
- Some gastrointestinal diseases – including Crohns disease.
- Some cholesterol lowering drugs (fibric acid derivatives e.g. Cliofibrate).
- Incidence of liver fluke is able to precipitate a particular type of pigmented gallstone and is relatively common in Asia (common especially if raw fish is regularly eaten).
- Food allergies are another trigger factor for gall related symptoms – if the gall is partly blocked consumption of food allergens trigger symptoms. The most common offenders are: egg, pork, onions/garlic, chicken, chocolate, dairy products chili, coffee, oranges, wheat, corn, beans and nuts in descending order. The high fat dairy products and pork are not recommended whether you have allergy/intolerance to them or not because of their saturated fat content.
- Coffee contracts the gall bladder – even if de-caffeinated – so if you have gallstones coffee may cause pain.
- Finally an odd one - sun-burning increases risk of gallstones.
Helpful Supplements and Nutritional Measures:
- Drink two large glasses of water on rising, and midmorning and mid afternoon to maintain the water content of the bile. Sliced un-peeled lemon in hot water is a bile stimulant too, and a healthy way to start the day. Add honey and some turmeric powder for anti-inflammatory benefits
- Take 2 fruits and 3 - 4 vegetable serves daily, especially including the cabbage family. This is for the fiber and important anti-oxidant content. (Carrots, beets, prunes, cabbage, broccoli, brussels sprouts, kiwi, papaya, apples are all very useful).
Lose excess weight (low animal fats and/or low sugar/sweets diet)
- Take extra mg vitamin C and 200 of vitamin E daily - improves bile solubility (Innate Response Antioxidant is our best antioxidant supplement)
- Fish oil ideally as 3 or 4 Krill Oil capsules daily (providing 750 - 1000mg of EPA and contains fat mobilizing phosphatidyl choline). We recommend this also for Fatty Liver. Oily fish include salmon, sardine, halibut herring, trout – twice or more weekly.
- Initially you need herbal bile stimulating herbs: Artichoke Extract is best and simplest for this, slightly lowering cholesterol and helping bowel movement along.
- Milk thistle can be used alternatively, having more benefits on detoxification and liver protection. A product giving Milk Thistle, Globe Artichoke and further nutrients as well (choline, methionine) called Liver Support – is often given for optimal liver-gall function.
- Exercising three times per week reduces gall stone formation.
- Take a probiotic - Lactobacilus bowel flora. These stimulate excretion of bile from the intestine, as well as binding these as well as other intestinal toxins and removing them.
Food Manufacturers Are Fooling You
Fact: The unhealthiest foods you could possibly eat often have the most health claims on the label. Ironic, isn't it? Think about most breakfast cereals. You're basically eating a bowl of sugar and flour. But the front of the box is packed with health claims:
- Low fat!
- Heart healthy!
- High fiber!
- Gluten-free!
- Reduced sodium!
- Made with whole grains!
Flip that box around like a smart grown-up and take a look at the ingredient list: sugar, flour, sugar in another form, sugar in a different color, sugar with a pretty name, etc. It's Type-2 diabetes in a bright box featuring a cartoon character selling love handles and loneliness.
And now they have a new marketing angle: a clever blend of childhood nostalgia and "fat acceptance." They tell us to eat what we want and love our body no matter what it looks like. Presumably, this is because they've finally recognized that the only people still eating cereal for breakfast have already given up on their health and body composition.
Funny thing is, when looking at the evidence, it's clear that there were never really health benefits in the first place to back up all these "healthy" labels. Here's how many of them originated and why they're wrong.
1 – Low Fat
It's taken over 40 years to officially call BS on the fraudulent claims about fat. The fear of dietary fat started in the 60's and 70's and immediately moved breakfast cereal into the "healthy" category. Hey, sugar is fat free! Bacon, eggs, and butter were out. Low-fat indigestible roughage was in because the research of the time was suggesting that saturated fat was clogging our arteries and increasing our risk of heart disease.
And despite the various top-notch review studies disproving this myth today, the cereal killers, sugar-water sellers, and big pharma phonies continue to lobby government officials, pay off medical and fitness professionals, and fund bogus research studies to keep it alive.
A low-fat diet isn't a benefit because eating fat doesn't cause disease. NOT eating it probably does, and we now know the body even needs some saturated fat to function optimally.
2 – High Fiber
Once you understand the origins of the low-fat guidelines it's easy to see how the advice to eat more fiber came about.
Denis Burkitt was the man behind the 1970's research linking high-fiber diets to lower rates of disease (colorectal cancer specifically). Just like Ancel Keys (the fat fraud), his evidence was awful. He basically claimed that African tribesman were healthier than Westerners because they ate their grains whole (with the fibrous outer shell). He conveniently failed to include a number of disease-free tribes thriving on starch-less diets high in saturated fat and animal protein, like the Masai.
Nonetheless, the bran we were throwing in the garbage became a prized possession, Burkitt wrote a best-selling book, and the "high-fiber" stamp fit perfectly next to the "low-fat" one on our breakfast bowl of blood sugar and body fat. It remains there today, right along with the misconception that whole grains are healthier than refined grains and that more fiber is a good thing, regardless of the source.
Meanwhile, the only study looking at the long-term impact of eating a high-fiber diet (DART, 1989) found an INCREASED risk of heart disease (23%) and mortality (27%). Those studies looking at colorectal cancer saw no benefit to upping our fiber intake:
"Our data do not support the existence of an important protective effect of dietary fiber against colorectal cancer or adenoma." (Fuchs CS et al. NEJM, 1999)
"In this large pooled analysis... high dietary fiber intake was not associated with a reduced risk of colorectal cancer." (Park Y et al. JAMA, 2005.)
3 – Cholesterol
The "lipid hypothesis" suggests that elevated cholesterol is associated with heart disease. And when we add it to what high-fiber, low-fat fanatics tell us, it's no wonder we think the way we do and fall for bogus health claims.
Right around the time all this low-fat, high-fiber evidence was surfacing, doctors and scientists were convinced they'd found the underlying cause of atherosclerosis – the narrowing and hardening of arteries. Nearly every doctor was on board with the theory. In the early 80's the National Institute of Health gathered 14 experts who voted unanimously that, "Lowering elevated blood cholesterol levels will reduce the risk of heart attacks caused by coronary heart disease."
They did so despite the fact that a causal relationship was never established, there's a library of evidence disproving it, and the original experiments used rabbits (herbivores that can't process dietary cholesterol) and a chemically prepared bare-cholesterol, which tends to oxidize.
But along came the prescription statins, and all of a sudden the questions and doctors aggressively opposing the theory disappeared. This created an environment where we dish out damaging side effects to more than 32 million Americans to lower the thing that's NOT associated with heart disease and does nothing to prevent it.
If cholesterol were associated with heart disease, there would be fewer heart attacks in those on statins and those with lower cholesterol, but there aren't. And there would be more heart attacks in those not on statins with higher cholesterol, but there aren't. The two variables aren't even related.
What we do see is statins causing mitochondrial and hormonal dysfunction, and lower cholesterol levels associated with cognitive and neurological impairment (Alzheimer's, Parkinson's, depression). This shouldn't come as a surprise when you understand that cholesterol is a building block for cell membranes, precursor to steroid hormones and essential nutrients, and fuel provider to neurons who can't generate it on their own.
"Our finding that low plasma cholesterol is associated with depressive symptoms in elderly men is compatible with observations that a very low total cholesterol may be related to suicide and violent death." (Morgan RE, et al. 1993, Lancet.)
Cereal fiber's ability to lower cholesterol is more of a detriment than a benefit. And realistically, the people getting heart attacks are the ones with elevated triglycerides, low HDL cholesterol, and excess small-dense (oxidizable) LDL particles – the same thing eating less saturated fat, more high-glycemic carbs, and vegetable oil-filled boxes of stuff claiming to "lower cholesterol" provides.
4 – Sodium
Heard the one about the obese, pre-diabetic guy with high triglycerides? Doc told him to eat less salt!
That's a joke. Or at least it should be. Salt doesn't make you fat and it's probably the last thing the average person needs to be worrying about when it comes to health.
High blood pressure is the fourth and final phase that turns Syndrome X into the Deadly Quartet. When you have metabolic syndrome, eating less salt won't do anything to solve the real problem.
- 2 weeks – insulin resistance (hyperinsulinemia)
- 2 months – elevated triglycerides (hyperlipidemia)
- 6 months – obesity (high bodyfat)
- 12 months – high blood pressure (hypertension)
People with high blood pressure don't need to eat less salt. They need to stop drinking liquid fructose and start driving-past instead of driving-thru.
More importantly, trying to abide by the FDA and AHA's recommendations to keep salt intake below 2400 mg per day (1tsp) increases cardiovascular disease risk and mortality from a heart attack or stroke. Ironically, this appears to be the result of elevated triglycerides and reductions in insulin sensitivity – the same thing driving the high blood pressure in the first place.
"The inverse association of sodium to CVD mortality seen here raises questions regarding the likelihood of a survival advantage accompanying a lower sodium diet." (Cohen HW, et al. AJM, 2006)
Therefore, one could say that your low-salt food is a double-whammy since you're consuming the food that's elevating the cause of high blood pressure and opting for the "lowers blood pressure" variety that's making it worse.
5 – Gluten
The gliadin proteins in wheat can be damaging to many people because of those proteins' ability to induce inflammation and increase intestinal permeability. Wheat itself may also cause cravings and interfere with your appetite-regulating mechanisms.
However, this doesn't mean all products with a "gluten-free" stamp of approval are suddenly health foods. Pizza is still pizza, pancakes are still pancakes, and a slab of pound cake beside your coffee is and always will be a bad choice... gluten-free or not. This should be common sense, but millions are willingly fooled every day because it's pretty easy to convince us that a delicious junk food is fine when it has an official-looking health claim on the box.
Just like we were tricked into selecting low-fat and low-sodium packaged products because of their apparent health benefit, food marketers have simply found another way to convince you that their bag or box of garbage is healthy.
Gluten-free cereal may be better than gluten-filled cereal, but it's still cereal. And you'd be better off leaving both for the birds.
References
- La Berg AF. 2008. How the Ideology of Low Fat Conquered America. J Hist Med Allied Sci 63(2):139-177.
- Siri-Tarino PW, et al. 2010. Meta-analysis of prospective cohort studies evaluating the association of saturated fat with cardiovascular disease. Am J Clin Nutr 91(3):535-46.
- Skeaff CM and Miller J. 2009. Dietary fat and coronary heart disease: summary of evidence from prospective cohort and randomised controlled trials. Ann Nutr Metab 55(1-3):173-201.
- Yamagishi K, et al. 2010. Dietary intake of saturated fatty acids and mortality from cardiovascular disease in Japanese: the Japan Collaborative Cohort Study for Evaluation of Cancer Risk (JACC) Study. Am J Clin Nutr 92(4):759-65.
- Mente A, et al. 2009. A systematic review of the evidence supporting a causal link between dietary factors and coronary heart disease. Arch Intern Med 169(7):659-69.
- Limb M. 2014. Tougher action is needed to address "alarming" levels of overweight and obesity, says England's chief medical officer. BMJ 348:g2438.
- Burkitt DP. 1971. Epidemiology of cancer of the colon and rectum. Cancer 28(1):3-13.
- Mann GV, et al. 1971. Atherosclerosis in the Masai. Am J Epidemiol 95 (1): 26-37.
- Burr ML, et al. 1989. Diet and reinfarction trial (DART): design, recruitment, and compliance. Eur Heart J 10(6):558-67.
- Fuch CS, et al. 1999. Dietary fiber and the risk of colorectal cancer and adenoma in women. N Engl J Med 340(3):169-76.
- Park Y, et al. 2005. Dietary Fiber Intake and Risk of Colorectal Cancer: A Pooled Analysis of Prospective Cohort Studies. JAMA 294(22):2849-2857.
- Steinberg D. 2006. Thematic review series: the pathogenesis of atherosclerosis. An interpretive history of the cholesterol controversy, part V: the discovery of the statins and the end of the controversy. J Lipid Res 47(7):1339-51.
- Kellner A. 1952. Lipid Metabolism and Atherosclerosis: The Ludwig Kast Lecture. Bull N Y Acad Med 28(1):11-27.
- Stehbens WE. 2001. Coronary heart disease, hypercholesterolemia, and atherosclerosis. I. False premises. Exp Mol Pathol 70(2):103-19.
- Golomb BA and Evans MA. 2008. Statin adverse effects : a review of the literature and evidence for a mitochondrial mechanism. Am J Cardiovasc Drugs 8(6):373-418.
- Krumholz HM, et al. 1994. Lack of Association Between Cholesterol and Coronary Heart Disease Mortality and Morbidity and All-Cause Mortality in Persons Older Than 70 Years. JAMA 272(17):1335-1340.
- Braunwald E. 1997. Cardiovascular Medicine at the Turn of the Millennium: Triumphs, Concerns, and Opportunities. N Engl J Med 337:1360-1369.
- Prior IA. 1981. Cholesterol, coconuts, and diet on Polynesian atolls: a natural experiment: the Pukapuka and Tokelau island studies. Am J Clin Nutr 34(8):1552-61.
- Superko HR, et al. 2002. Small LDL and its clinical importance as a new CAD risk factor: a female case study. Prog Cardiovasc Nurs 17(4):167-73.
- Kendrick M. 2007. The Great Cholesterol Con: The Truth About What Really Causes Heart Disease and How to Avoid It. John Blake.
- Corona G, et al. 2010. The effect of statin therapy on testosterone levels in subjects consulting for erectile dysfunction. J Sex Med 7(4 Pt 1):1547-56.
- West R, et al. 2008. Better memory functioning associated with higher total and low-density lipoprotein cholesterol levels in very elderly subjects without the apolipoprotein e4 allele. Am J Geriatr Psychiatry 16(9):781-5.
- Huang X, et al. 2008. Low LDL cholesterol and increased risk of Parkinson's disease: prospective results from Honolulu-Asia Aging Study. Mov Disord 23(7):1013-8.
- de Lau LM, et al. 2006. Serum cholesterol levels and the risk of Parkinson's disease. Am J Epidemiol 164(10):998-1002.
- Shin JY, et al. 2008. Are cholesterol and depression inversely related? A meta-analysis of the association between two cardiac risk factors. Ann Behav Med 36(1):33-43.
- Perez-Rodriguez MM, et al. 2008. Low serum cholesterol may be associated with suicide attempt history. J Clin Psychiatry 69(12):1920-7.
- Seneff S. 2009. APOE-4: The Clue to Why Low Fat Diet and Statins may Cause Alzheimer's
- Morgan RE, et al. 1993. Plasma cholesterol and depressive symptoms in older men. Lancet 341(8837):75-9.
- Brown L, et al. 1999. Cholesterol-lowering effects of dietary fiber: a meta-analysis. Am J Clin Nutr 69(1):30-42.
- Swain JF, et al. 1990. Comparison of the Effects of Oat Bran and Low-Fiber Wheat on Serum Lipoprotein Levels and Blood Pressure. N Engl J Med 322:147-152.
- Barnard RJ, et al. 1998. Diet-induced insulin resistance precedes other aspects of the metabolic syndrome. J Appl Physiol 84(4):1311-1315.
- Alderman MH, et al. 1998. Dietary sodium intake and mortality: the National Health and Nutrition Examination Survey (NHANES I). 351(9105):781-785.
- Jurgens G and Graudal NA. 2003. Effects of low sodium diet versus high sodium diet on blood pressure, renin, aldosterone, catecholamines, cholesterols, and triglyceride. Cochrane Database Syst Rev 1:CD004022.
- Garg R. 2011. Low-salt diet increases insulin resistance in healthy subjects. Metabolism 60(7):965-968.
- Cohen HW, et al. 2006. Sodium Intake and Mortality in the NHANES II Follow-up Study. Am J Med 119(3):275e7-275e14.
- Fasano A, et al. 2003. Prevalence of celiac disease in at-risk and not-at-risk groups in the United States: a large multicenter study. Arch Intern Med 163(3):286-92.
- Troncone R and Jabri B. 2011. Coeliac disease and gluten sensitivity. J Intern Med 269(6):582-590.
- Fasano A. 2011. Zonulin and its regulation of intestinal barrier function: the biological door to inflammation, autoimmunity, and cancer. Physiol R 91(1):151-75.
- Fasano A. 2012. Zonulin, regulation of tight junctions, and autoimmune diseases. Ann N Y Acad Sci 1258(1):25-33.
Grains - The Real Cereal Killer
By Dr. Mercola
The persistent myth that dietary fat causes obesity and promotes heart disease has undoubtedly ruined the health of millions of people. It's difficult to know just how many people have succumbed to chronic poor health from following conventional low-fat, high-carb recommendations, but I'm sure the number is significant.
In the featured documentary, Cereal Killers, 41-year-old Donald O'Neill turns the American food pyramid upside-down—eliminating sugars and grains, and dramatically boosting his fat intake. In so doing, he improves his health to the point of reducing his hereditary risk factors for heart disease to nil.
Watching people's reactions to his diet brings home just how brainwashed we've all become when it comes to dietary fat. Most fear it. Yet they will consume sugar in amounts that virtually guarantee they'll suffer all the devastating health consequences they're trying to prevent by avoiding fat, and then some!
Fat versus Carbs—What Really Makes You Pack on the Pounds?
The fact is, you've been thoroughly misled when it comes to conventional dietary advice. Most dietary guidelines have been massively distorted, manipulated, and influenced by the very industries responsible for the obesity epidemic in the first place—the sugar and processed food industries.
Shunning the evidence, many doctors, nutritionists, and government health officials will still tell you to keep your saturated fat below 10 percent, while keeping the bulk of your diet, about 60 percent, as carbs.1 This is madness, as it's the converse of a diet that will lead to optimal health.
A recent Time Magazine2 article highlighted a report by the Environmental Working Group (EWG), which showed that many breakfast cereals contain more than 50 percent sugar by weight! Cereals marketed specifically to children are among the worst offenders. Kellogg's Honey Smacks and Mom's Best Cereals Honey-Ful Wheat topped the list with 56 percent sugar by weight. If you're looking for alternatives for your family you could try Snackimals from Barbara's. Snackimals is not on the EWG's list because it is a newer product. All of their flavors have only 7 grams of sugar per serving.
Even diabetes organizations promote carbohydrates as a major component of a healthy diet—even though grains break down to sugar in your body, and sugar promotes insulin resistance, which is the root cause of type 2 diabetes in the first place.
As noted in the film: "If we could get all diabetics to eat a high-fat, high-protein, low-carbohydrate diet, we would cut the insulin requirement so dramatically that it's been estimated that six pharmaceutical companies would go out of business tomorrow."Contrary to popular belief, you do not get fat from eating fat. You get fat from eating too much sugar and grains.
Refined carbohydrates promote chronic inflammation in your body, elevate low-density LDL cholesterol, and ultimately lead to insulin and leptin resistance. Insulin and leptin resistance, in turn, is at the heart of obesity and most chronic disease, including diabetes, heart disease, cancer, and Alzheimer's—all the top killers in the US.
Don't Fear the Fat
In the film, O'Neill switches over to a diet where 70 percent of his calories come from healthy fat—most of it in the form of macadamia nuts (my personal favorite)—and the remaining 30 percent of his caloric intake is divvied up between protein and fibrous fruits and vegetables. Over the course of 28 days, O'Neill:
- Loses weight and body fat
- Increases his lean muscle mass
- Feels more energetic and improves his athletic performance
- Increases his resting metabolic rate
- Improves his blood pressure, cholesterol, and other measurements to the point that he no longer has any risk factors for heart disease, which he's genetically predisposed for
Of particular importance here is that O'Neill's total cholesterol and LDL levels wentup, which initially caused significant concern. However, once they tested the LDL particle numbers, the results showed that his LDL particles were the largest species known, and he had virtually no small LDL particles at all.
This is phenomenal, as it's the small, dense LDL particles that cause inflammation. Large particles do not. Also, the markers for inflammation were virtually nonexistent, showing that he has no inflammation in his body at all. All in all, his one-month long high-fat, no-carb diet experiment proved that:
- Eating fat helps you lose fat
- Eating saturated fat decreases your risk factors for heart disease
- Regardless of your genetic predisposition your diet is, ultimately, the determining factor
I would also add that his results show the benefits of a high-fat, low-carb diet for athletes, many of whom are still convinced that this type of diet will make them heavy and sluggish. On the contrary, O'Neill breaks his own athletic record during his experiment, and refers to his renewed sense of vigor as feeling like a "spring lamb."
This high and sustained energy is a hallmark of ketogenesis, where your body is burning fat rather than sugar as its primary fuel. When your body burns fat, you don't experience the energy crashes associated with carbs.
Saturated Fat and Cholesterol Are Both Necessary for Optimal Health
Contrary to popular belief, saturated fats from animal and vegetable sources provide a number of important health benefits, and your body requires them for the proper function of your:
Cholesterol—another wrongly vilified dietary component—also carries out essential functions within your cell membranes, and is critical for proper brain function and production of steroid hormones, including your sex hormones. Vitamin D is also synthesized from a close relative of cholesterol: 7-dehydrocholesterol.
Your body is composed of trillions of cells that need to interact with one another. Cholesterol is one of the molecules that allow for these interactions to take place. For example, cholesterol is the precursor to bile acids, so without sufficient amounts of cholesterol, your digestive system can be adversely affected. It's also critical for synapse formation in your brain, i.e. the connections between your neurons, which allow you to think, learn new things, and form memories. In fact, there's reason to believe that low-fat diets and/or cholesterol-lowering drugs may cause or contribute to Alzheimer's disease.3
Replacing Refined Carbs with Healthy Fat—The Answer to Most of Your Health Concerns
Underlying most chronic diseases, including obesity, type 2 diabetes, heart disease, and cancer are inflammation and insulin/leptin resistance. When you eat carbohydrates, your blood sugar, insulin, and leptin will all temporarily rise, and these spikes are very pro-inflammatory. Where you have inflammation, disease and dysfunction follows. An excellent editorial in the journal Open Heart4 reviews the cardiometabolic consequences of replacing saturated fats with carbohydrates, which includes the following:
The answer, then, lies in avoiding these inflammatory spikes in blood sugar, insulin and leptin, and reversing insulin and leptin resistance. To do this, you need to:
- Avoid refined sugar, processed fructose, and grains. This means avoiding processed foods, as they are chockfull of these ingredients, along with other chemicals that can wreak metabolic havoc
- Eat a healthful diet of whole foods, ideally organic, and replace the grain carbs you cut out with:
- Moderate amounts of high-quality protein from organic, grass-fed or pastured animals (this is to ensure you're not getting the antibiotics, genetically engineered organisms, and altered nutritional fat profile associated with factory farmed animals)
- High amounts of high-quality healthful fat as you want (saturated and monounsaturated). Many health experts now believe that if you are insulin or leptin resistant, as 85 percent of the US population is, you likely need anywhere from 50 to 85 percent of your daily calories in the form of healthful fats for optimal health. Good sources include coconut and coconut oil, avocados, butter, nuts (particularly macadamia), and animal fats. Avoid all trans fats and processed vegetable oils (such as canola and soy oil). Also take a high-quality source of animal-based omega-3 fat, such as krill oil.
- As many vegetables as you can muster. Juicing your vegetables is a good way to boost your vegetable intake
Another "add-on" suggestion is to start intermittent fasting, which will radically improve your ability to burn fat as your primary fuel. This too will help restore optimal insulin and leptin signaling.
What's the Deal with Protein?
Dr. Rosedale, who was one of my primary mentors on the importance of insulin and leptin, was one of the first professionals to advocate both a low-carb and moderate protein (and therefore high-fat) diet. This was contrary to most low-carb advocates who were, and still are, very accepting of using protein as a replacement for the carbs.
The problem is that, along with grains, most Americans tend to eat far too much protein. While your body certainly has a protein requirement, there's evidence suggesting that eating more protein than your body needs could end up fueling cancer growth.
Dr. Rosedale advises limiting your protein to one gram of protein per kilogram of lean body mass (or 0.5 grams per pound of lean body weight). For most people, this means cutting protein down to about 35-75 grams per day. Pregnant women and those working out extensively need about 25 percent more. I believe this theory is worthy of consideration. The key though is to add healthy fat to replace the carb and protein calories you're cutting out of your diet. Again, sources of healthy fat include:
Your Health Is Within Your Control
Groundbreaking research by the likes of Dr. Robert Lustig and Dr. Richard Johnson (author of the books, The Sugar Fix and The Fat Switch) clearly identifies the root cause of obesity, diabetes, heart disease, and numerous other chronic diseases, and it's notfat. It's refined sugar—particularly fructose—consumed in excessive amounts. Their research, and that of others, provides us with a clear solution to our current predicament. In short, if you want to normalize your weight and protect your health, you need to address your insulin and leptin resistance, which is the result of eating a diet too high in sugars and grains.
For a comprehensive guide, see my free optimized nutrition plan. Generally speaking though, you'll want to focus your diet on whole, ideally organic, unprocessed or minimally processed foods. For the best nutrition and health benefits, you'll also want to eat a good portion of your food raw.
Sugar is highly addictive, and if you're like most people, you're no stranger to carb cravings. Just know that once your body gets used to burning fat instead of sugar as its primary fuel, those cravings will vanish. Many cereals and other grain products would not be quite as harmful if they didn't also contain so much added sugar. Even many organic brands contain excessive amounts. This is unfortunate, since many (Americans in particular) are really indoctrinated to eat cereal for breakfast. I've been working on a low-sugar cereal line for some time now, to provide a healthier alternative for those who really don't want to give up their breakfast cereal. I hope to have it ready sometime this summer.
Last but not least, for those of you still concerned about your cholesterol levels, know that 75 percent of your cholesterol is produced by your liver, which is influenced by your insulin levels. Therefore, if you optimize your insulin level, you will automatically optimize your cholesterol, thereby reducing your risk of both diabetes and heart disease.
Also, remember that even if a high-fat, low-carb diet was to raise your total cholesterol and LDL, it doesn't automatically mean that your diet is increasing your risk factors for heart disease. As O'Neill did in this film, you need to test your LDL particle number. Large-sized particles are good, while the smaller, denser particles can penetrate the lining of your arteries and stimulate the plaque formation associated with heart disease. The former does NOT increase your heart disease risk, while the latter one will. To learn more about LDL particle numbers and how to test them, please see my previous interview with Chris Kresser, L.Ac., which goes into this in some detail.
Too Much Protein??
Media sources often report, “too much protein stresses the kidney.” What does science say? Martin and colleagues reviewed the available evidence regarding the effects of protein intake on kidney function with a particular emphasis on kidney disease. The researchers found: “Although excessive protein intake remains a health concern in individuals with preexisting renal disease, the literature lacks significant research demonstrating a link between protein intake and the initiation or progression of renal disease in healthy individuals.” In addition “At present, there is not sufficient proof to warrant public health directives aimed at restricting dietary protein intake in healthy adults for the purpose of preserving renal function.” Protein restriction is common treatment for people with kidney problems.
Protein: The Facts, the Myths, and the Real Science
Everyone has an opinion about protein, and the myths surrounding it are rampant. That's why sorting the facts from the crap will lead to better choices regarding your own diet and protein intake. Answer the questions below and see if you've been falling for the myths.
Fact or Myth?
The RDA (Recommended Dietary Allowance) protein suggestions are just fine for people who work out.
Hint: The RDA guideline for protein is 0.8 grams per kilogram of bodyweight per day. So if you weigh 190 pounds (86 kilograms) you'd need about 69 grams of protein.
The Answer: Lifters and athletes concerned with their performance or physique require more protein than what's recommended by the RDA. So it's a myth (and a joke) that the RDA protein recommendations are adequate for ass-kicking individuals.
Here's Why: RDA protein recommendations are too low for certain groups. Those recommendations were never intended for people attempting to enhance performance, maintain, or gain muscle. In fact, a higher protein intake may have positive benefits regarding different health ailments including obesity, type 2 diabetes, osteoporosis, heart disease and muscle wasting.
The RDA guideline reflects the minimum daily needs of protein required to maintain short-term nitrogen balance in healthy, moderately active people. Nitrogen balance compares the amount of nitrogen coming into the body (from dietary protein) to the amount being lost. It's often used as a measurement of protein balance since protein is 16 percent nitrogen.
If you're consuming the same amount of nitrogen that you're losing, you're in nitrogen balance. If you're consuming more than you're losing, you're in positive nitrogen balance. If you're losing more than you're consuming, you're in negative nitrogen balance and are losing protein.
Nitrogen balance studies often involve examining urinary nitrogen levels. Approximately 90 percent of the nitrogen in urine is urea and ammonia salts – the end products of protein metabolism. The remaining nitrogen is accounted for by other nitrogen-containing compounds.
This nitrogen balance method is useful, but it has problems: Urine collections tend to underestimate nitrogen losses, dietary intake tends to be overestimated, miscellaneous skin and hair losses are prone to error, and the response to increased protein intake varies tremendously.
The Really Geeky Stuff
- In a review published in the International Journal of Sports Nutrition, researchers concluded, "Those involved in strength training might need to consume as much as 1.6 to 1.7 grams of protein per kilogram per day (approximately twice the current RDA) while those undergoing endurance training might need about 1.2 to 1.6 grams per kilogram per day (approximately 1.5 times the current RDA)."
- In another article published in Nutrition & Metabolism, researcher Donald Layman argued that the dietary guidelines should be improved and reflect new understandings about protein requirements. According to him, "During the past decade a growing body of research reveals that dietary protein intakes above the RDA are beneficial in maintaining muscle function and mobility." Diets with increased protein have been shown to improve adult health when it comes to treatment or prevention of obesity, type 2 diabetes, osteoporosis, heart disease and muscle wasting.
- A review published in the International Journal of Sport Nutrition and Exercise Metabolism was conducted to evaluate the effects of dietary protein on body composition in energy-restricted resistance-trained athletes, and to provide protein recommendations for these athletes.
The researchers concluded that "...the range of 2.3 to 3.1 grams per kilogram of FFM (fat free mass) is the most consistently protective intake against losses of lean tissue." In other words, for every kilogram on your body that's not fat, you should be consuming 2-3 grams of protein in order to preserve lean tissue. So if you have 190 pounds of lean tissue, up to 258 grams of protein would be optimal for you.
In addition, the goal of the athlete should be considered. Leaner athletes or those having a primary goal of maintaining maximal FFM should aim toward intakes approaching the higher end of this range. Even higher levels of protein than those recommended in the review are not uncommon in exercising individuals. It's unlikely that negative health consequences will follow from higher levels of intake, assuming there are no related health problems that would suggest limiting intake.
Fact or Myth?
The thermic effect of protein is the same as it is for carbs and fat.
Hint: The thermic effect of feeding or diet induced thermogenesis (DIT) is the amount of energy your body has to expend in order to digest and assimilate food. So picture a lean chicken breast (mostly protein), a bowl of rice (mostly carb), and tablespoon of butter (mostly fat). Which do you think your body will have to work hardest to digest?
The Answer: Among the three macronutrients, protein ranks highest in diet induced thermogenesis. So it's a myth that they're all equal in terms of their thermic effect. That means it'll cost you more calories to digest and absorb protein than it would fat and carbohydrate.
Here's Why: The consumption of protein requires an expenditure of 20-30% of the calories derived from protein. So, if 200 calories of protein are eaten, 40-60 calories are burned during digestion. DIT from carbohydrate is 15-20% and 2-5% for fat.
Fact or Myth?
Protein is more satiating (filling) than fat or carbohydrate.
Hints: Protein has an influence on CCK (cholecystokinin) and ghrelin. Protein may stimulate cholecystokinin (CCK) and decrease ghrelin. CCK is secreted mostly from the inner layer of the gastrointestinal tract has been shown to act as a satiety signal. The satiating effect of CCK was first demonstrated when administering CCK to rats. It "dose dependently" reduced meal size. Ghrelin is produced primarily in the stomach and has appetite increasing properties. Ghrelin levels are relatively high prior to a meal and they decrease after a meal.
The Answer: It's a fact that protein is usually more satiating than fat or carbs. When comparing protein, fat, and carbohydrate, protein is generally reported as the most satiating (satisfying to a point of full or beyond) and fat as the least satiating.
Here's Why: Research indicates that one of the primary factors involved with the satiating effects of protein is the thermic effect of feeding, mentioned above. Though protein's influence on ghrelin and CCK may play a large role in its satiating effects, more research needs to be conducted in these areas, as findings have been indecisive. Future research should concentrate on different levels of protein, different types of protein, and consumption of proteins in short and long term.
The Really Geeky Stuff
- A review published in Nutrition & Metabolism reported that protein induced thermogenesis has an important effect on satiety. "Protein plays a key role in body weight regulation through satiety related to diet-induced thermogenesis."
- A study published in Physiology & Behavior investigated the relative satiating effect of the macronutrients in lean women. On four separate occasions, the composition of an iso-caloric lunch "preload" was controlled in 12 lean women. Macronutrient composition had a significant effect on short-term hunger – the women were less hungry after the protein preload compared to the preloads with the other macronutrients. They also ate less after the protein preload.
- A study published in the American Journal of Clinical Nutrition tested the prediction that increasing protein while maintaining the carb content of a diet lowers body weight due to decreased appetite and decreased calorie intake. The study showed when increasing the protein intake from 15% of diet to 30% of diet (while eating the same amount of carbs) there was a decrease in appetite and fewer calories were consumed.
- The Journal of Clinical Endocrinology & Metabolism published a study that compared the effect of different proteins and carbohydrates on indicators of appetite and appetite regulatory hormones. CCK level was one of the primary outcomes measured.
Calorie intake was higher after the glucose preload compared with lactose and protein preloads. CCK level was higher 90 minutes after the protein preloads compared with glucose and lactose level. Researchers concluded that "acute appetite and energy intake are equally reduced after consumption of lactose, casein, or whey compared with glucose."
One Quick Caveat
The research sometimes gets a little messy. For example, some studies are indecisive when it comes to protein intake and ghrelin levels. This is why you need to rely on your own reasoning, logic, and experience while gathering info from the research.
References
- Blom, A.M., Lluch, A., Stafleu, A., Vinoy, S., Holst, J., Schaafsma, G., & Hendriks, H. (2006). Effect of high-protein breakfast ont he postprandial ghrelin response. The American Journal of Clinical Nutrition, 83(2), 211-220.
- Bowen, J., Noakes, M., Trenerry, C., & Clifton, P.M. (2006).Energy intake, Ghrelin, and Cholecystokinin after Different Carbohydrate and Protein Preloads in Overweight Men. The Journal of Clinical Endocrinology & Metabolism, 91(4).
- Helms, E., Zinn, C., Rowlands, D.S., & Brown, S.R. (2014). A Systematic Review of Dietary Protein During Caloric Restriction in Resistance Trained Lean Athletes: A Case for Higher Intakes. International Journal of Sport Nutrition and Exercise Metabolism, 24, 127-138.
- Layman, D.K.(2009). Dietary Guidelines should reflect new understandings about adult protein needs. Nutrition & Metabolism, 6(12), Lemon, P. (1998). Effects of exercise on dietary protein requirements. International Journal of Sports Nutrition, 8(4), 426-447.
- Lucas, M, & Heiss C.J.(2005) Protein needs of older adults engaged in resistance training: A review. Journal of Aging and Physical Activity, 13(2), 223-236.
- Moran, L.J., Luscombe-Marsh, N.D., Noakes, M., Wittert, G.A., Keogh, J.B., & Clifton, P.M. (2005). The Satiating Effect of Dietary Protein Is Unrelated to Postprandial Ghrelin. The Journal of Clinical Endocrinology & Metabolsim, 90(9).
- Poppitt, S.D., McCormack, D., & Buffenstein, R. (1998).Short-term effects of macronutrient preloads on appetite and energy intake in lean women. Physiology & Behavior, 64(3), 279-285.
- Weigle, D.S., Breen, P.A., Matthys, C.C., Callahan, H.S., Meeuws, K.E., Burden, V.R., & Purnell, J.Q. (2005). A high-protein diet induces sustained reductions in appetite, ad libitum caloric intake, and body weight despite compensatory changes in diurnal plasma leptin and ghrelin concentrations. The American Journal of Clinical Nutrition, 82(1), 41-48.
- Westerterp, K.R. (2004). Diet induced thermogenesis. Nutrition & Metabolism, 1, 1-5
What Enzymes Does Mercury Inhibit?
Mercury is a heavy metal that has been used for centuries as a medicine and a poison. Common exposures come from contaminated seafood, dental amalgams, and vaccines for infants. Mercury can exist in 11 different chemical states or compounds. At the molecular level, it forms bonds with sulfhydryl groups on an enzyme, which are parts of the enzyme that contain a sulfur atom that is attached to a hydrogen atom (SH). Binding of mercury can change the shape of the enzyme and block its activity. Enzymes inhibited by mercury include acetylcholinesterase, catalase, dipeptyl peptidase (CD26), amylase, lipase, lactase and glucose-6-phosphatase.
Acetylcholinesterase
Acetylcholine is one of the main neurotransmitters that nerves use to control muscle movement. After release, acetylcholine must be degraded in order to stop the “go” signal from continuing to stimulate the receiving cell. Acetylcholine is degraded by an enzyme called acetylcholinesterase. This enzyme is found in the synaptic cleft, which is the space between the "fingertips" of a nerve cell and the neighboring cell that the nerve activates. Mercury inhibits this enzyme differently in different species, depending on whether it can easily find a sulfhydryl group to latch onto. For human acetylcholinesterase, it takes millimolar amounts of mercuric chloride (HgCl2) to inhibit the enzyme.
Catalase
Catalase is an enzyme that converts hydrogen peroxide into water and oxygen. Hydrogen peroxide is regularly produced by cells as they make energy in a process called cellular respiration. Hydrogen peroxide is toxic at high levels, so cells get rid of it via the enzyme catalase. Though it is widely known that mercury inhibits catalase, it may do so by binding to sites other than sulfhydryl groups. It is interesting to note that when a person absorbs elemental mercury, which causes brain damage, catalase is the enzyme in the red blood cells that converts elemental mercury into an ionic form (mercuric salt).
Creatine Kinase
Mercury also inhibits the enzyme found in skeletal muscle called creatine kinase. Muscle cells contract by using an energy molecule called adenosine triphosphate (ATP), a molecule with three -- thus the “tri” prefix -- phosphates. Energy is released for an enzyme when the enzyme grabs ATP and breaks off one phosphate, resulting in adenosine diphosphate (ADP) -- “di” means two. A quick way of making ATP is to take a phosphate from a sugar molecule called phosphocreatine and add it to ADP. Creatine kinase is the enzyme that recharges ADP into ATP in this way. Mercury inhibits creatine kinase in several ways. Mercury blocks creatine kinase’s ability to bind ADP or the magnesium ion that the enzyme needs in order to function properly.
Digestive Enzymes
Mercury binds to sulfhydryl groups, which is found on the amino acid cysteine. Since cysteine is a common amino acid in many enzymes, mercury inhibits a whole host of enzymes. The "Journal of Applied Toxicology" reported the effects of inorganic mercury in the liver tissue of freshwater fish. Mercury inhibited many enzymes involved in digestion of food molecules, such as protein, carbohydrate and fat: amylase, lipase, lactase and maltase. Mercury also inhibited glucose-6-phosphatase, an enzyme involved in the production and export of glucose in cells.