Why We Need to Supplement
The word is out—it pays to take your vitamins.
In 2002, the American Medical Association (AMA) reversed its long-held anti-vitamin stance and began to encourage all adults to supplement daily with a multi-vitamin. A landmark review of 38 years of scientific evidence by Harvard researchers, Dr. Robert Fletcher and Dr. Kathleen Fairfield convinced the conservative Journal of the American Medical Association (JAMA) to rewrite its policy guidelines regarding the use of vitamin supplements. In two reports, published in the June 19, 2002 edition of JAMA, the authors concluded that the current US diet, while sufficient to prevent acute vitamin deficiency diseases, such as scurvy and pellagra, is inadequate to support long-term health.
Insufficient vitamin intake is apparently a cause of chronic diseases. Recent evidence has shown that suboptimal levels of vitamins (below standard), even well avocet those causing deficiency syndromes, are risk factors for chronic diseases such as cardiovascular disease, cancer and osteoporosis. A large portion of the general population is apparently at increased risk for this reason. — Dr. Fletcher and Dr. Fairfield
In the study, the authors examined several nutrients, including vitamins A, B6, B12, C, D, E, K, folic acid and several of the carotenoids (including alpha and beta carotene, cryptoxanthin, zeaxanthin, lycopene and lutein). Among their conclusions, they noted:
- folic acid, vitamin b6 and B12 are required for proper homocysteine metabolism, and low levels of these vitamins are associated with increased risk of heart disease (homocysteine is a sulphur-containing amino acid that, at high blood levels, can damage the cardiovascular system);
- inadequate folic acid status increases the risk of neural tube defects and some cancers (a neural tube defect is an incomplete closing of the spinal cord that occurs early in fetal development);
- vitamin E and lycopene (the red pigment found in ripe tomatoes) appears to decrease the risk of prostate cancer;
- vitamin D is associated with a decreased risk of osteoporosis and fracture when taken with calcium (osteoporosis is a hollowing out of the bones caused by the loss of calcium);
- inadequate vitamin B12 is associated with anaemia and neurological disorders (anaemia is a decrease in number of red blood cells or a lack of hemoglobin in the blood);
- low dietary levels of carotenoids, the brightly colored pigments in peppers, carrots and fruits, appear to increase the risk of breast, prostate and lung cancers (carotenoids belong to the family of nutrients called bioflavonoids);
- inadequate vitamin C is associated with increased cancer risk; and
- low levers of vitamin A are associated with vision disorders and impaired immune function
In a striking departure from JAMA’s long held anti-vitamin stance, the authors concluded that, given our modern diet, supplementation each day with a multi-vitamin is a prudent preventive measure against chronic disease. The researchers based their guidance on the fact that more than 80% of the American population does not consume anywhere near the five servings of fruits and vegetables required each day for optimal health.
JAMA’s previous comprehensive review of vitamins, conducted in the 1980’s, concluded that people of normal health do not need to take a multivitamin and can meet all their nutritional needs through diet alone. Since that time, nutritional science has compiled an impressive wealth of studies affirming the health benefits of supplementation as an adjunct to a healthy diet. The American Medical Association’s about-face in light of the Fairfield-Fletcher studies, and its public declaration that supplementation is now deemed important to your health, underscores the strength of the scientific evidence that now prevails.
The Case for Supplementation
We now have convincing evidence that the lifetime risk of cancer; heart disease; stroke; diabetes; neurological disorders, such as multiple sclerosis and amyotrophic lateral sclerosis (Lou Gehrig’s disease); macular degeneration; osteoporosis; Alzheimer’s disease and other forms of dementia can be reduced by providing the cells of the body with sufficient amount of the right nutrients.
One of the first human studies to substitute the benefits of vitamin supplements was announced in 1992 and showed that men who took 800 mg/day of vitamin C lived six years longer than those who consumed the US Food and Nutrition Board’s recommended daily allowance of 60 mg/day. Published in the journal Epidemiology, this ten year follow-up study showed that high vitamin C intake extended average lifespan and reduced mortality from both cardiovascular disease and cancer.
A compelling report that high-potency supplements extend human lifespan was published in August 1996, in the American Journal of Clinical Nutrition. The study involved 11,178 elderly people who participated in trial to establish the effects of vitamin supplements on mortality. Supplementation with vitamin E, alone, reduced the risk of overall mortality by 34% and reduced the risk of coronary disease mortality by 47%. However, when vitamin C and E were used together, overall mortality was reduced by 42% and coronary mortality dropped by 53%, demonstrating the synergistic effects of multiple vitamin therapy. What made these findings of even greater significance was that the study compared people who took low potency one-a-day multivitamins to those who took higher potency vitamin C and E supplements. Only those participants taking high-dose vitamin C and E supplements benefitted.
A 1997 study published by the British Medical Journal evaluated 1,605 healthy men with no evidence of pre-existing heart disease. Those men deficient in vitamin C were found to have a 350% increased incidence of sudden heart attacks compared to those who were not deficient in vitamin C. The authors concluded that vitamin C deficiency, as measure by low blood levels of ascorbate, is a significant risk factor for coronary heart disease.
A massive cohort study, published in 1998, investigated the risk for colon cancer in 88,756 nurses who took folic acid (a B-complex vitamin) as part of a daily multivitamin supplement.
The study found that intakes of 400 mg/day or more of folate, compared to intakes of 200 mg/day or less, were strongly related to lowered risk. While no significant protective effects were noted over shorter periods, an inverse relationship between folate intake and cancer risk became apparent after five years of use. After 15 years, a remarkable 75%reduction in the risk of colon cancer was noted among those women taking the supplements containing the B-complex vitamin. The authors concluded that longterm use of multivitamins might substantially reduce the risk for colon cancer, an effect likely related to the folic acid contained in these products.
In this same study, nurses who took multivitamins containing vitamin B6 also reduced their risk of heart attack by 30%. The evidence revealed that the more vitamin B6 they took, the lower the risk was of suffering a sudden cardiac event. These finding support those of another cohort study conducted in Norway that demonstrated a combination of folic acid and vitamin B6 can reduce homocysteine levels by up to 32% in healthy individuals. Homocysteine, a harmful amino acid at high blood levels, can markedly increase the level of inflammation and oxidative stress in blood vessels, which can precipitate both heart attack and stroke.
In 2005, an international coalition led by Canadian researchers at McMaster University, Ontario, provided evidence that a comprehensive ‘cocktail’ of nutritional supplements can significantly improve lifespan in animal models. The nutrient mixture, containing 31 nutrients common to many better quality broad-spectrum supplements available on the market, targeted key factors in the again process, including the proliferation of reactive oxygen species (ROS aka free radicals), inflammatory processes, insulin resistance and mitochondrial dysfunction. In the study, the treatment group of mice exhibited an 11% increase in lifespan compared to normal mice who did not receive the supplement cocktail. Previously, the same researcher established that the supplement cocktail completely abolished severe cognitive decline expressed by aging untreated mic. The results from these animal-model experiments demonstrate that broad-spectrum dietary supplements may be effective in ameliorating the effects of again and age-related pathologies where simpler formulation have generally failed.
The benefits of supplementation with n-3 polyunsaturated fatty acids (omega-3 fats) after a heart attack are well documented. Omega-3 fatty acids, commonly found in cold-water fish, nuts and grains, dramatically reduce the risk of premature death in high-risk individuals. A 2008 study on post-myocardial infarction (heart attack) patients revealed a significantly lowered likelihood of dangerous cardiac arrhythmia and an 85% reduction in the risk of premature death by simply maintain an optimal level of omega-3 fats in the diet. Moreover, these protective effects are also seen in healthy populations. In healthy people with no evidence of heart disease, men and women appear to achieve the same level of protection against premature death by supplementing with omega-3 oils from fish and nuts. In a 2010 Norwegian study, elderly men with no evidence of overt heart disease who supplemented with fish oil experience a 47% reduction in the risk of premature death compared to those who did not supplement. Similarly, a large Australian study found that women with the highest levels of omega-3 consumption from nuts and fish had a 44% reduction in the risk of premature death from inflammatory disease. The protective effect was dose-related to the level of omega-3 intake. The ability of omega-3 fats to reduce the level of systemic inflammation through the production of anti-inflammatory prostaglandins (primitive cell signaling hormones) appears to be the source of their protective talents.
A 19-year study of colorectal cancer rates found the relative risk in men with poor vitamin D status was almost triple that of men with sufficient vitamin D. In a meta-analysis conducted on research worldwide from 1966 to 2004, researchers from the University of California concluded that 1,000 IU/day of vitamin D lowers an individual’s risk of developing colorectal cancer by as much as 50%. A 2006 review of vitamin D status and cancer risk in the northeastern United States concluded that efforts to improve vitamin D status through vitamin D supplementation could markedly reduce cancer incidence and mortality at low cost and with few or no adverse effects. A 2008 review of current research findings on the cancer-protective effects of vitamin D concluded that intakes of between 1000 and 4000 IU per day protect against cancers of the breast, colon, prostate, ovary, lungs and pancreas. Lastly, a 2009 review on ultraviolet radiation, vitamin D and cancer concluded that circulating levels of vitamin D play an important role in determining the outcomes of several cancers. According to the authors of this review, support for the sunlight/vitamin D/cancer link is scientifically strong enough to warrant the use of vitamin D in cancer prevention and treatment protocols.
These studies and their finding are but a few of the thousands of independent scientific reports confirming the efficacy of supplementation with high quality nutritional supplements as a prudent, preventative measure for optimal health and disease prevention.
The Other Side of the Coin
To be certain, the premise of life extension and disease prevention through supplementation does not have universal support amongst the scientific community. As is inevitably the case, in an evidence based discipline there will arise conflicting studies that cast doubt on the evidence. Many researchers argue that supplements provide a convenient and effective means for supplying the optimal intakes of essential nutrients required to support long-term health; others counter that there is no conclusive proof that supplements provide any real health benefits at all.
Unfortunately, much of the debate is framed by a media more interested in selling newspapers than in ferreting out the truth. Sloppy reporting, distorted editorial sensationalism, and conflicts of interest by researchers and publishers have unnecessarily alarmed the public and have treated to destroy its trust in complementary health care. Health conscious consumers and medical practitioners alike have become frustrated at the mixed messages promulgated through the headlines: one day we are told something is good for us and the next day we are told it is bad for us. Why do so many recently published studies appear to refute the prevailing scientific evidence about the benefits of natural approaches to wellness? How can vitamin E be good for us one day and bad for us the next? For once, why can’t the experts just get it straight?
If it is of any consolation, it may be helpful to understand that science never progresses smoothly—there will always be new findings that appear to refute long established theories. Controversy is the crucible for change and paves the road that science must travel to arrive at a final truth. Unfortunately, media bias and conflicts of interest place unnecessary detours along the way.
Firstly, the consumer must understand that out of 100 clinical studies that investigate a particular effect, probability dictates that five of these studies—no matter how well designed—will show results that are not real. There will always be a statistical fluke in the bunch.
Secondly, about one-fifth of clinical trials investigating a particular effect will not have the needed number of subjects to show a statistically significant result. This occurs because in most clinical trials the probability of finding a real result, known as the power of a test, is set at a minimum of 80%. Consequently, there is up to a 20% chance of missing your mark and failing to find a different when one actually exists. This is merely the gremlin of probability at work.
Thirdly, some investigations are just bad science, improperly conducted, poorly reported and inadequately reviewed. Unfortunately, as has been the case in several recent studies, their findings attract an inordinate amount of attention from a media hungry for headlines.
Except from NutriSearch's Comparative Guide to Nutritional Supplements, 5th Professional Edition.
Questions Concerning Soy Safety
While there are those out there who continue to praise soy as some kind of miracle food, evidence continues to emerge which exposes its many faults and raises questions about its safety.
Soy and other foods and herbs with estrogen-mimicking properties are often recommended to menopausal and post-menopausal women because high consumption may lead to amelioration of some of the symptoms associated with the natural decline in estrogen levels. They are also sometimes included in protocols designed to reduce the effects of excess estrogen in women with “estrogen dominance” and elevated levels of the estrogen fractions associated with higher rates of breast cancer. Phytoestrogens bind to estrogen receptors in the human body, thereby blocking the binding of the body’s natural estrogen. And since these plant estrogens have a much milder effect than true estrogen, they are believed to help with some of the symptoms associated with excess estrogen. Soy seems to play both sides of the coin: it has estrogenic effects, but can also be used to lessen estrogenic effects. Head spinning yet? Perhaps this is why the results of studies looking at soy and female health are so mixed.
Soy is also touted as a good source of protein, because it is one of the only complete proteins among plant foods (meaning it contains all the essential amino acids; although like all legumes, it is low in methionine). However, what is often not mentioned in the same sentence when soy is being touted as a plant-based protein source is that soy is also notorious for interfering with digestion of the very protein it provides. Soy contains trypsin inhibitors—compounds that reduce the efficacy of digestive enzymes—and these hardy anti-nutrientswithstand a high level of processing, so they’re still present in most commercial soy foods.
While Asian diets—commonly cited for being more health-promoting than Western diets—do contain soy products, they are usually prepared by traditional fermentation methods that reduce the potency of the digestive inhibitors and anti-nutrients. Moreover, soy sauce, miso, natto, and edamame are consumed in small quantities, and sometimes only as a garnish. Soy consumption in Asia is a world apart—no pun intended—from soy consumption in the modern United States, where vegetarians and vegans following plant-based diets can sometimes be better referred to as “soytarians.” They consume unprecedented amounts of soy, largely in the form of highly refined, puffed, extruded, and otherwise processed foods, such as soy milk, soy-based breakfast cereal, soy “chicken,” soy “cheese,” textured vegetable protein, and other soy-based foods marketed as imitation meat and dairy products.
Adults who have made a deliberate decision to consume a lot of soy aren’t the only ones affected by soy’s potentially adverse effects. With 25% of infant formula in the U.S. being soy-based, developing babies can be unwitting participants in an experiment that may have negative consequences for their long-term health.
A recent study sheds light on a possible connection between increased seizure rates in autistic children fed soy formula, as compared to those fed dairy formulas. The author also found an association between soy formula consumption and epilepsy. The study identified a comorbidity of autism and epilepsy of 1.6–3.8%, which is higher than in the general population. Within that, among soy-fed infants there was a 3.6% rate of epilepsy, which is over twice as high as the 1.7% among non-soy fed infants. These numbers might seem very small, but as the author points out, “These may be considered by some readers as small percentages in each group who had seizures, but the two-fold or greater differences between soy and non-soy diets are statistically significant. Pharmaceutical interventions that reduced the incidence of febrile seizures or epilepsy by 2-fold would be in demand.”
It’s important to note that these were associations, and they do not necessarily imply causality. However, similar findings relate soy consumption to seizures in other populations, as shown in an animal model of neurological diseases. Nevertheless, although the study was small and retrospective, it raises concerns which, when combined with other studies that sound the alarm, suggest people should be more cautious when ingesting large amounts of soy products that may have adverse effects on the body’s endocrine and neurological functions—particularly in populations as vulnerable as developing infants.
For more information check out the Whole Soy Story
Calcium Supplements May Damage the Heart
After analyzing 10 years of medical tests on more than 2,700 people in a federally funded heart disease study, researchers at Johns Hopkins Medicine and elsewhere conclude that taking calcium in the form of supplements may raise the risk of plaque buildup in arteries and heart damage, although a diet high in calcium-rich foods appears be protective.
In a report on the research, published Oct. 10 in the Journal of the American Heart Association, the researchers caution that their work only documents an association between calcium supplements and atherosclerosis, and does not prove cause and effect.
But they say the results add to growing scientific concerns about the potential harms of supplements, and they urge a consultation with a knowledgeable physician before using calcium supplements. An estimated 43 percent of American adult men and women take a supplement that includes calcium, according the National Institutes of Health.
“When it comes to using vitamin and mineral supplements, particularly calcium supplements being taken for bone health, many Americans think that more is always better,” says Erin Michos, M.D., M.H.S., associate director of preventive cardiology and associate professor of medicine at the Ciccarone Center for the Prevention of Heart Disease at the Johns Hopkins University School of Medicine. “But our study adds to the body of evidence that excess calcium in the form of supplements may harm the heart and vascular system.”
The researchers were motivated to look at the effects of calcium on the heart and vascular system because studies already showed that “ingested calcium supplements — particularly in older people — don’t make it to the skeleton or get completely excreted in the urine, so they must be accumulating in the body’s soft tissues,” says nutritionist John Anderson, Ph.D., professor emeritus of nutrition at the University of North Carolina at Chapel Hill’s Gillings School of Global Public Health and a co-author of the report. Scientists also knew that as a person ages, calcium-based plaque builds up in the body’s main blood vessel, the aorta and other arteries, impeding blood flow and increasing the risk of heart attack.
For more information be sure to look at the article on Johns Hopkins Medical site.
The Plastic Plague
Each day we encounter well over 500 chemicals that our bodies are tasked with detoxifying. Some of the worst and most pervasive are Phthalates that not only are instrumental in causing allergies but have been linked to prostatic hypertrophy, endometriosis, breast cancer, hypo-testosteronism, hypothyroidism, infertility, animals mating with the same sex, inability to lose weight, asthma, birth defects, cancers, diabetes, and infinitely more. Phthalate levels in the human body are over 10,000 times higher than most other pollutants. No other pollutant even comes close!
Let's take a look at just one toxic environmental chemical family that is in all of us. We literally cannot avoid it if we live on this planet. U.S. Government researchers have found them in all humans. Even when researchers drop helicopters into pristine road-less areas, far from industry, they find this pollutant in all species of life they examine, from fish and salamanders to the largest mammals. They are actually a family of man-made chemicals which define modern life as we know it, the phthalates, better recognized by you as plastics and plasticizers. But they go far beyond our concept of a plastic, because they add flexibility, durability, slow-release, cost-effectiveness, scent, light and heat protection, and many other properties to things we do not consider as plastics.
Phthalates (plastic-derived carcinogenic chemicals made from petroleum) are in your plastic water bottle and other food containers (linings of cans, juice boxes, plastic wrap and Styrofoam trays), not to mention infant formula bottles. In fact baby bottles have some of the highest levels of phthalates, and this is made even worse by microwaving a baby's bottle. Plus when the mother drinks out of plastic water bottles, the plastics cross the placenta and head for the fetus's brain and glands that produce hormones. And unfortunately low doses have been shown to be more toxic than higher ones. Phthalates are in food containers of nearly every type from soup to cereals, hidden in boxes, bags and beer, food and soda cans, or blatantly in Styrofoam trays and cups and plastic wrap, and plastic bottles and jugs. Phthalates are in dental fillings (composites), even the glues for dental crowns, the bags that hold "safe" saline breast implants, and are a large part of dental implants and joint replacement adhesives or glues and elute from coronary artery stents (methylacrylates).
Phthalates or plasticizers outgas from IVs, dental materials, vinyl floors, carpeting, mattresses, most furnishings (couches, chairs, mattresses, desk and tables), appliances, computers, home and office and construction materials, automobiles, the coatings of electric wires (nestled in the walls of every building outgas as they heat), PVC plumbing, etc. The list is endless. Clearly phthalates are the most ubiquitously unavoidable pollutant in the human body. The evidence is overwhelming. The phthalates (plastics) permeate every aspect of our life, since they are ingredients in even cosmetics and toiletries, nail polishes, perfumes, deodorants, hair conditioners, lotions and other personal care products as well as medications, especially those that are called "extended release" or "24 hour" or "time release" or "slow release". For it is the plastic coating that creates this property.
And if these were not dangerous enough by themselves, they are never alone. They are usually combined in products with equally or even more dangerous environmental pollutants like the phthalate cousin BPA (bisphenol A, often accompanies phthalates), PBDE (flame retardants), PFOA (stain resistant, water resistant, Teflon type chemicals), VOHs (volatile organic hydrocarbons which include xylene, toluene, benzene, and hundreds more), pesticides, etc. All these are often called POPs, or persistent environmental pollutants, because most of them take decades to break down.
And now even animals in the wild have measurable levels in their systems. Yet they don't use Styrofoam cups, plastic water and infant bottles, nor shrink-wrap their foods in plastic. Nor do they live in enclosed homes and offices with huge amounts of furnishings as well as appliances that outgas phthalates. Nor do they ride in toxic car/planes, in heavy exhaust, or work in polluted factories and offices made from an abundance of construction materials making them literal phthalate cocoons. We have truly changed the air on the planet Earth in this century. And worse, we have changed the chemistry of the human body more than at any other time.
The evidence now for phthalates being able to contribute to or directly causing every malady known is overwhelming. Babies are born with measurable levels, and if they have to spend time in the hospital to be on IVs, or have catheters or gastric tubes, this raises their levels even further. Birth defects and lowered IQ, hypothyroidism, neurologic and especially brain dysfunctions are among the many spin-off diseases from the privilege of living in this world of convenient plastics. Cancers, from prostate, testicular and breast to brain and pancreatic, can be programmed in the genetic of babies while they are still in the womb, only to have their emergence suppressed until adulthood.
In many of the reports you will encounter the term bisphenol A or BPA. As a broadly used industrial chemical and polycarbonate and epoxy resin that also lines food cans, BPA migrates directly form those containers into the foods, just as phthalates do. Although BPA is not technically a phthalate, it is most of the time found combined with phthalates (from carbonless copy paper to cabinets) and his its own toxic properties in addition to those of the phthalates that it's connected with. Therefor since these two toxins are usually present as a combination, it is quite meaningless to separate their toxicities since they usually occur in combination. As well, they share several mechanisms of toxicity in the body. So don't be hoodwinked by proclamations that a products is "BPA free". The manufacturers assume you are ignorant of the hidden phthalates.
Meanwhile, remember phthalates and BPA are only two thousands of chemicals that we are exposed to and minimally hundreds each day that our bodies are asked to detoxify. Even chemicals in cellophane and plastic windows of cookie boxes are proven to migrate into the foods that they do not even contact. We cannot escape them, nor can we detoxify or metabolize all that we are exposed to in a day.
Excerpt from "How to Cure Diabetes!" by Sherry Rogers
Smart Abdominal Training
Although you are regularly bombarded with exercises claiming to tone and strengthen the abdominal muscles, many of these exercises are inadequate and ineffective. Some exercises may actually lead to lower back pain, and do little to strengthen the abdominals.
The ‘villains’ of abdominal training are the hip flexors, which bring the legs and trunk toward each other. Muscles that flex the hip include the psoas major, illiacus, rectus femoris, pectineus and sartorius. Full sit-ups involve the hip flexors, which may cause the lower back to arch and unwanted back pain, particularly in individuals with relatively weak abdominals. Leg-raising exercises in a supine position challenge the hip flexors with limited involvement of the abdominals. Frequently, there is a muscle imbalance between the weaker abdominals and the stronger hip flexors in trunk flexing movements. The goal of abdominal training is to maximize the involvement of the abdominals, while minimizing the involvement of the hip flexors.
How to Fix Anterior Pelvic Tilt
Importance of Structural Balance for Injury Prevention
What is the Science Behind Structural Balance Assessments?
The concept of structural balance is that a muscle’s ability to develop force is a function of the strength of the opposing muscle group and its stabilizers. Many training and sports-related injuries are often the result of muscular imbalances – strength discrepancies between opposing and synergist muscle groups or even between limbs. These structural imbalances are often caused by a combination of the repetitive motions involved in many sports and/or a lack of exercise variety in training.
A Structural Balance Analogy:
Another way to understand structural balance to imagine you are building a house. In construction, the term “footing” describes the concrete support that the foundation is built upon. The footing also spreads the weight of the structure evenly over a wider area. The walls of the house are then built on the foundation. However, if the footing is poorly developed it compromises the stability of the foundation, which in turn, compromises the structural integrity of the entire house.
Each of the body’s joints are similar to the above analogy in that the joint is the house and the muscles and tendons controlling that joint are the foundation and footing. Viewed as a whole, if the stability of one joint is compromised it will affect the structural integrity of the entire body.
This is the proverbial “only as strong as the weakest link” axiom.
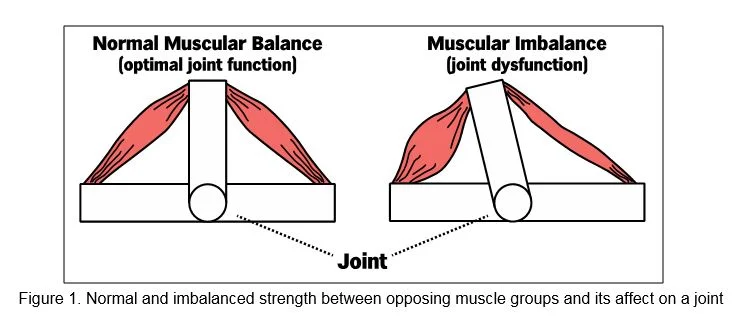
A joint is controlled by two primary sets of opposing muscle groups; one set of muscles flexes the joint and the other extends it. Synergistic muscles help the respective primary muscle perform its action. While one primary muscle group and its synergists are moving the joint, the opposing muscle group and it synergists are stabilizing it from the opposite side.
There is an optimal balance of strength between these muscle groups that control a joint, but if the muscles on one side of the joint are disproportionately stronger than the muscles on the opposing side it creates joint instability, which increases the risk of injury to that joint.
The take away point here is balance is important and vital to injury prevention.
Figure 1: Notice the difference between normal and imbalanced strength and its impact on a joint.
When the central nervous system senses joint instability, it reduces the ability to continue strengthening the muscles that are already too strong. This an effective safety mechanism the body utilizes to protect itself from injury.
However, this safety mechanism can be “overridden” by attempting to force the already too strong muscles to get even stronger — many injuries occur under these conditions. If you place more strain on the weakest link than it can tolerate, the chain breaks.
While unpredictable accidents will still occur, a thorough structural balance assessment can:
- Identify muscle weaknesses that leave a joint vulnerable to injury and compromise performance;
- Faulty movement patterns that cause misalignment of the body, which results in distorted movement;
- Muscle tightness that can result in strained or torn muscles, and;
- Provide the blueprint from which your initial training program is developed.
A structural balance assessment also provides a starting point for your training. Your initial training program is developed based on the results of your assessment and aimed at correcting your weaknesses, faulty movement patterns, and tight muscles through a progression of corrective and remedial exercises. This approach expedites your results and helps ensure continuous progress.
A thorough structural assessment should be the first step of anyone’s training program whether you are a competitive athlete from any level of competition, an avid CrossFitter, or someone who wants to look better and improve your health.